What is ovarian cancer? What causes it, what are the symptoms, what’s the treatment and how can you prevent it? This feature by Healthline explores and answers these questions for you:
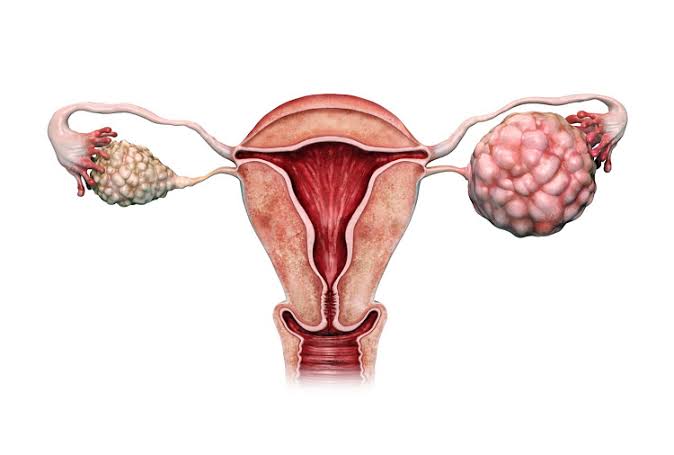
The ovaries are small, almond-shaped organs located on either side of the uterus. Eggs are produced in the ovaries. Ovarian cancer can occur in several different parts of the ovary.
Ovarian cancer can start in the ovary’s germ, stromal, or epithelial cells. Germ cells are the cells that become eggs. Stromal cells make up the substance of the ovary. Epithelial cells are the outer layer of the ovary.
Early stage ovarian cancer may not have any symptoms. That can make it very difficult to detect. However, some symptoms may include:
- frequent bloating
- quickly feeling full when eating
- difficulty eating
- a frequent, urgent need to urinate
- pain or discomfort in the abdomen or pelvis
These symptoms have a sudden onset. They feel different from normal digestion or menstrual discomfort. They also don’t go away.
Other symptoms of ovarian cancer can include:
- lower back pain
- pain during intercourse
- constipation
- indigestion
- fatigue
- a change in the menstrual cycle
- weight gain
- weight loss
- vaginal bleeding
- acne
- back pain that worsens
If you have these symptoms for longer than two weeks, you should seek medical attention.
Researchers do not yet understand what causes ovarian cancer to form. Different risk factors can increase a woman’s chances of developing this type of cancer, but having those risk factors doesn’t mean you will develop the cancer.
Fibroids: Causes, symptoms, types, diagnosis, treatment
Cancer forms when cells in the body start growing and multiplying abnormally. Researchers studying ovarian cancer are trying to identify which genetic mutations are responsible for the cancer.
These mutations may be inherited from a parent or they can also be acquired. That is, they occur during your lifetime.
Epithelial carcinoma of the ovary
Epithelial cell carcinoma is the most common type of ovarian cancer. It makes up 85 to 89 percent of ovarian cancers. It’s also the fourth most common cause of cancer death in women.
This type often doesn’t have symptoms in the early stages. Most people aren’t diagnosed until they’re in the advanced stages of the disease.
Genetic factors
This type of ovarian cancer can run in families and is more common in women who have a family history of:
- ovarian cancer and breast cancer
- ovarian cancer without breast cancer
- ovarian cancer and colon cancer
Women who have two or more first-degree relatives, such as a parent, sibling, or child, with ovarian cancer are at the highest risk. However, having even one first-degree relative with ovarian cancer increases the risk. The “breast cancer genes” BRCA1 and BRCA2 are also associated with ovarian cancer risk.
Factors that are linked to increased survival
Several factors are linked to increased survival in women who have epithelial carcinoma of the ovary:
- receiving a diagnosis at an earlier stage
- being a younger age
- having a well-differentiated tumor, or cancer cells that still closely resemble healthy cells
- having a smaller tumor at the time of removal
- having a cancer caused by BRCA1 and BRCA2 genes
Germ cell cancer of the ovary
“Germ cell cancer of the ovary” is a name that describes several different types of cancer. These cancers develop from the cells that create eggs. They usually occur in young women and adolescents and are most common in women in their 20s.
These cancers can be large, and they tend to grow quickly. Sometimes, tumors produce human chorionic gonadotropin (HCG). This can cause a false-positive pregnancy test.
Germ cell cancers are often very treatable. Surgery is the first-line treatment. Chemotherapy after the surgery is highly recommended.
Stromal cell cancer of the ovary
Stromal cell cancers develop from the cells of the ovaries. Some of these cells also produce ovarian hormones including estrogen, progesterone, and testosterone.
Stromal cell cancers of the ovaries are rare and grow slowly. They secrete estrogen and testosterone. Excess testosterone can cause acne and facial hair growth. Too much estrogen can cause uterine bleeding. These symptoms can be quite noticeable.
This makes stromal cell cancer more likely to be diagnosed at an early stage. People who have stromal cell cancer often have a good outlook. This type of cancer is usually managed with surgery.
Treatment for this cancer depends on the type, stage, and whether you want to have children in the future.
Surgery
Surgery can be done to confirm the diagnosis, determine the stage of the cancer, and potentially remove the cancer.
During surgery, your surgeon will try to remove all tissue that contains cancer. They may also take a biopsy to see if the cancer has spread. The extent of the surgery may depend on whether you want to be pregnant in the future.
If you want to become pregnant in the future and you have stage 1 cancer, surgery can include:
- removal of the ovary that has cancer and a biopsy of the other ovary
- removal of the fatty tissue, or omentum attached to some of the abdominal organs
- removal of abdominal and pelvic lymph nodes
- biopsies of other tissues and collection of fluid inside of the abdomen
Advanced ovarian cancer surgery
Surgery is more extensive if you don’t want to have children. You also may need more surgery if you have stage 2, 3, or 4 cancer. Complete removal of all areas involved with cancer may prevent you from becoming pregnant in the future. This includes:
- removal of the uterus
- removal of both ovaries and fallopian tubes
- removal of the omentum
- removal of as much tissue that has cancer cells as possible
- biopsies of any tissue that might be cancerous
Chemotherapy
Surgery is usually followed by chemotherapy. Medications can be given intravenously or through the abdomen. This is called intraperitoneal treatment. Side effects of chemotherapy can include:
- nausea
- vomiting
- hair loss
- fatigue
- problems sleeping
Treatment of symptoms
While your doctor prepares to treat or remove the cancer, you may need additional treatment for the symptoms the cancer is causing. Pain is not uncommon with ovarian cancer.
The tumor can put pressure on nearby organs, muscles, nerves, and bones. The larger the cancer, the more intense the pain may be.
Pain may also be a result of treatment. Chemotherapy, radiation, and surgery can leave you in pain and discomfort.
Diagnosing this cancer starts with a medical history and physical exam. The physical exam should include a pelvic and rectal examination. One or more blood tests may also be used to diagnose this condition.
An annual pap smear test does not detect this cancer. Tests that may be used to diagnose this cancer include:
- a complete blood count
- a test for cancer antigen 125 levels, which may be elevated if you have ovarian cancer
- a test for HCG levels, which may be elevated if you have a germ cell tumor
- a test for alpha-fetoprotein, which may be produced by germ cell tumors
- a test for lactate dehydrogenase levels, which may be elevated if you have a germ cell tumor
- a test for inhibin, estrogen, and testosterone levels, which may be elevated if you have a stromal cell tumor
- liver function tests to determine if the cancer has spread
- kidney function tests to determine if the cancer has obstructed your urine flow or spread to the bladder and kidneys
Other diagnostic studies can also be used to check for signs of ovarian cancer:
Biopsy
A biopsy is essential for determining if cancer is present. During the procedure, a small tissue sample is taken from the ovaries to look for cancer cells.
This can be done with a needle that’s guided by a CT scan or by an ultrasound. It can also be done through a laparoscope. If fluid in the abdomen is present, a sample can be examined for cancer cells.
Imaging tests
There are several types of imaging tests that can look for changes in the ovaries and other organs that are caused by cancer. These include a CT scan, MRI, and PET scan.
Checking for metastasis
If your doctor suspects ovarian cancer, they may order other tests to see if the cancer has spread to other organs. These tests may include the following:
- A urinalysis can be done to look for signs of infection or blood in the urine. These can occur if cancer spreads to the bladder and kidneys.
- A chest X-ray can be done to detect when tumors have spread to the lungs.
- A barium enema can be done to see if the tumor has spread to the colon or rectum.
Regular cancer screenings are not recommended. Right now, medical experts believe they return too many false results. However, if you have a family history of breast, ovarian, fallopian tube, or peritoneal cancer, you may want to be tested for certain gene mutations and be screening regularly.
While a cause for ovarian cancer is not known, researchers have identified several risk factors that may increase your risk for developing this type of cancer. They include:
- Genetics: If you have a family history of ovarian, breast, fallopian tube, or colorectal cancer, your risks for developing ovarian cancer are higher. That’s because researchers have identified certain genetic mutations that are responsible for these cancers. They can be passed from parent to child.
- Personal medical history: If you have a personal history of breast cancer, your risk for ovarian cancer is higher. Likewise, if you’ve been diagnosed with certain conditions of the reproductive system, your odds of developing ovarian cancer are higher. These conditions include polycystic ovary syndrome and endometriosis, among others.
- Reproductive history: Women who use birth control actually have a lower risk of ovarian cancer, but women who use fertility drugs may have a higher risk. Likewise, women who’ve been pregnant and breastfed their infants may have a lower risk, but women who’ve never been pregnant are at an increased risk.
- Age: Ovarian cancer is most common in older women; it’s rarely diagnosed in women under age 40. In fact, you’re more likely to be diagnosed with ovarian cancer after menopause.
- Ethnicity: Non-Hispanic white women also have the highest risk of ovarian cancer. They’re followed by Hispanic women and black women.
- Body size: Women with a body mass index over 30 have a higher risk for ovarian cancer.
The stage of ovarian cancer is determined by three factors:
- the tumor’s size
- whether or not the tumor has invaded tissues into the ovary or nearby tissues
- whether or not the cancer has spread to other areas of the body
Once these factors are known, cancer of the ovary is staged according to the following criteria:
- Stage 1 cancer is confined to one or both ovaries.
- Stage 2 cancer is confined to the pelvis.
- Stage 3 cancer has spread into the abdomen.
- Stage 4 cancer has spread outside of the abdomen or into other solid organs.
Within each stage are substages. These substages tell your doctor a bit more about your cancer. For example, stage 1A ovarian cancer is cancer that has developed in just one ovary. Stage 1B cancer is in both ovaries.
Survival rates are an indication of how many people with the same type of cancer are alive after a specific period of time. Most survival rates are based on five years. While these numbers do not tell you how long you may live, they do provide an idea of how successful treatment for a particular type of cancer is.
For all types of ovarian cancer, the five-year survival rate is 47 percent. However, if ovarian cancer is found and treated before it spreads outside the ovaries, the five-year survival rate is 92 percent.
However, less than one quarter, 15 percent, of all ovarian cancers are found at this early stage.
This cancer rarely shows symptoms in the early stages. As a result, it’s often not discovered until it has progressed into advanced stages. There’s currently no way to prevent this cancer, but doctors know of factors that lower your risk of developing ovarian cancer.
These factors include:
- taking birth control pills
- having given birth
- breastfeeding
- tubal ligation (also known as “getting your tubes tied”)
- hysterectomy
Tubal ligation and hysterectomy should only be performed for valid medical reasons. For some, a valid medical reason may be reducing your risk of ovarian cancer. However, you and your doctor should discuss other prevention options first.
You should talk to your doctor about early screening for ovarian cancer if you have a family history of it. Specific gene mutations can put you at risk for ovarian cancer later. Knowing if you have these mutations can help you and your doctor stay vigilant for changes.
The prognosis for people diagnosed with ovarian cancer depends on how advanced the cancer is when it’s discovered and how well treatments work. Early stage 1 cancers have a better prognosis than late stage ovarian cancers.
However, only 15 percent of ovarian cancers are discovered in the initial stage. More than 80 percent of women with ovarian cancer are diagnosed when the cancer is in an advanced stage.
While the ovaries may be just one organ, more than 30 types of ovarian cancer exist. They’re classified by the type of cell where the cancer begins, plus the stage of the cancer.
The most common type of this cancer is epithelial tumors. More than 85 percent of this cancer first develops in the cells that are lining the outer portion of the ovaries.
One in 78 women will be diagnosed with this cancer in their lifetimes. Older women are more likely to be diagnosed with ovarian cancer. The average age for an ovarian cancer diagnosis is 63 years old.
Only 15 percent of these cancer cases are diagnosed in the early stage.
Women whose cancer is diagnosed in an early stage have a five-year-survival rate of 92 percent. For all types and stages of cancer, the five-year relative survival rate is 47 percent.